TEXGHS partners from around the world develop complementary innovations
Since its early formation in March of last year, Texas Global Health Security Innovation Consortium (TEXGHS) has been hard at work, bringing together medical personnel, public health institutions, and innovators and professionals within academia, public and private sectors to create and fund solutions to fight this pandemic and future ones.
TEXGHS partners have been developing solutions for many of the problems that local, state and federal public health agencies in the nation and world face against COVID-19, and in many cases, these innovations fit like puzzle pieces and could work in tandem to solve various issues plaguing the globe. For example, a combination of Epistemix, Vaccine Systems and Ocean Process creates a complete solution for public authorities during the COVID-19 pandemic. The package includes the safe occupancy of educational and governmental buildings, local vaccine production from vaccine manufacturers, and vaccine administration management including priority lists, tracking brands and documenting possible side effects.
With a vast history in the infectious disease space, one such company is leveraging a digital twin of the US population that includes each individual, schools, workplaces, hospitals and other information to model and simulate scenarios to show decision makers the probable impacts of various policies and choices to help them create better futures. Based out of Pittsburgh, Epistemix is utilizing this information to help officials make informed decisions about COVID-19, using its software known as FRED (Framework for Reconstructing Epidemiological Dynamics).
“We’re looking at improving public health, improving the conditions for people to live better lives, and making sure policies that are governing populations of people … are pointing to outcomes that are good for society,” said John Cordier, CEO and co-founder of Epistemix.
The software is very flexible, and Cordier said it can be used to model any number of conditions that arise in a population. The emergence of COVID-19, however, has shifted the team’s focus solely to the pandemic. Using their software to run simulations of the pandemic under different policy scenarios, Epistemix maps the spread of the pandemic in various regions across the country, determines the threshold needed for vaccination coverage, and examines the level of immunity reached in each region based on the natural history of COVID-19, vaccination allocation strategies and other policies.
“What we’re doing with our platform is enabling people to make better choices to improve the health of communities and populations across the U.S.,” Cordier said. “Decision makers … (are) asking questions like, ‘What if we open schools this way? What if we have events of this size under this level of immunity in the population?’ And we’re able to look at how those choices and decisions impact the future that they’re creating.”
By utilizing data from multiple sources across the U.S., Epistemix has created a synthetic population or a digital twin of U.S. society which can be used in different ways to model the outcome of social dynamics and choices. States are beginning to implement this technology and reaping the benefits.
“(People) can better understand the impact that each of the strategies they’re considering would have based on the stage of the epidemic,” Cordier said.
For example, with the roll out of vaccines, the software can determine the number of doses needed to serve the population for each distribution center, how that allocation strategy impacts the epidemic moving forward, and any gaps that occur during vaccine deployment, Cordier said.
“Based on that information, we can put that into the platform and forecast going forward what’s the level of immunity achieved in that particular area,” Cordier said. “And once that level of immunity goes over that threshold, things are safe to open up. But until that point, you have to have a balance of having things open or still wearing masks, et cetera.”
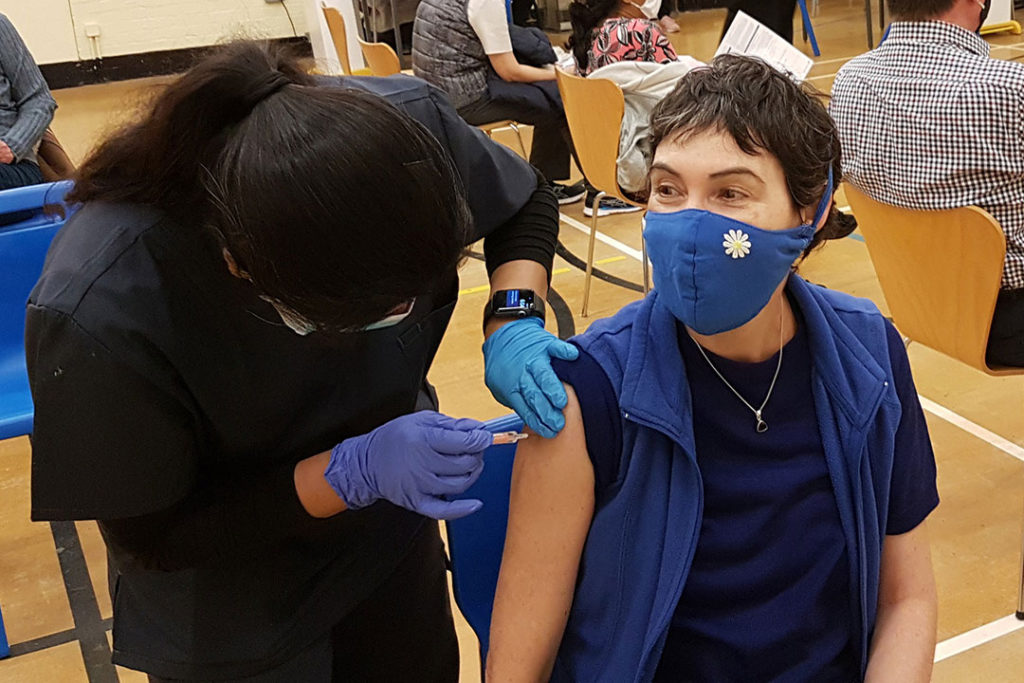
As the worst surge yet of COVID-19 overwhelms healthcare systems worldwide, health professionals, government officials and the media worry a COVID-19 vaccine is not being deployed quickly enough. Another company developing a COVID-19 solution that directly addresses this challenge is Vaccine Systems. Its answer – a device that speeds the processing of vaccines at the point of care, helping ensure accuracy, reducing wastage, and simplifying the preparation of vaccines for frontline healthcare workers – ultimately saving lives.
The device, known as the Automated Vaccine Reconstitution System (AVRS), mixes vaccine with a fluid called diluent in a process called reconstitution. Today, this is a slow cumbersome manual process that needs to be completed at the point of care, one factor in the slow deployment of the Pfizer COVID-19 vaccine.
“Our system reduces to a single tap of a touchpad what are normally nine cumbersome manual steps to reconstitute or mix a vaccine,” said Bob LiVolsi, CEO of Vaccine Systems. “It’s fast, accurate and safe.”
In 2018, LiVolsi began his company after noticing many issues associated with vaccines requiring reconstitution. He discovered that during a mass vaccination campaign in Sierra Leone, 750,000 people came to get vaccinated for yellow fever, but 250,000 were turned away. Yellow fever vaccine requires reconstitution.
“There were 250,000 doses wasted – that went unused and thrown away, so it made no sense,” LiVolsi said. “I found some documentation from Doctors Without Borders where on an internal issue brief they said, ‘Half of the vaccines requiring reconstitution, which represent about half of the vaccines administered, were being wasted’.”
If 1,000 people were to visit a vaccination center, and the vaccine was prepared ahead of time, there is a specific timeframe within which it can be injected, LiVolsi said. If it is reconstituted too early or too late, this leads to wastage.
This reconstitution of a single vial can take an experienced person approximately three minutes to complete. AVRS can speed up the process exponentially, especially in mass campaigns with people lined up for vaccination.
“Our system mixes five vials of vaccine in about a minute and a half, at least ten times faster than the manual process,” LiVolsi said. “For example, AVRS can mix 25 doses of the Pfizer vaccine in 90 seconds whereas it can take up to 15 minutes manually. That improvement allows you to have vaccine ready quickly or ‘just-in-time’ rather than making vaccine ahead of time and risking wastage.”
AVRS also effectively eliminates human error during the reconstitution process, potentially saving lives. In 2018, nurses administering measles vaccine inadvertently used the wrong diluent, killing two children in American Samoa. This frightened the population, and rather than vaccinating at the region’s historic 90% rate, they vaccinated for measles at a 34% rate. LiVolsi said, “It resulted in another 100 people dying from measles, and 6,000 people getting it in a very small population.”
Vaccine System’s device prevents this with scanners that, before reconstituting, read the vials to make sure the diluent and vaccine match. This feature could have prevented the deadly outbreak in American Samoa. It could also have stopped the inadvertent administration of antibodies instead of COVID-19 vaccine to 44 people in West Virginia in late December 2020.
“For a parent concerned about vaccine safety, knowing that a vaccine is mixed right and that their child isn’t vulnerable to somebody having a bad day and making an error in preparing a vaccine, or vulnerable to a healthcare worker just overwhelmed by the intense activity of a pandemic – this should be reassuring,” LiVolsi said. “It could be the kind of thing which pushes a vaccine hesitant person from being reluctant to vaccinate their child to have enough confidence to vaccinate.”
The device is currently in development. Vaccine Systems hopes to deploy the technology at vaccination sites this summer.
Across the globe in Denmark, a company called Ocean Process is developing a platform to stop the spread of the coronavirus and help with vaccine management and contact tracing.
“Everybody is focusing so much on vaccination to pave our way forward, but it won’t solve the COVID problem until half a year from now,” said Kaare Nørgaard, founder and CEO of Ocean Process. “Vulnerable groups will be protected, so it won’t be as bad as it used to be, but stopping the disease will require a longer haul of vaccinations, and we can’t wait for that.”
The company’s solution – Cure GPS – which was created in partnership with NNIT and can help contact tracers effectively reach more people.
“The problem about COVID and all this contact tracing is whenever you reach out to a contact of (someone infected), they will already have been infected and contagious for a while, so you actually also need to reach their contacts,” said business partner Christian Drejøe. “Part of our hypothesis is that if you actually go out that extra level, you can stop the chain of transmission.”
Cure GPS notifies people if they have been in contact with someone who tested positive for COVID-19, provides information about what to do if so, and follows up with individuals, inviting them to add the contact information for the people they have been in contact with. Drejøe said the amount of work a contact tracer does tracing five people is the same amount of work the platform can do tracing 30 individuals.
“Now we have contacted on average 30 people, but on average only one person has been infected,” Drejøe said. “As soon as we find out who that is, then the contact tracers will contact those five, and the rest will be released in the workflow. They will automatically get a text message (saying), ‘You do not have to worry. The person we thought was sick is not sick’.”
Because test results typically take about two to three days to receive, the 25 individuals in the workflow will only have had to quarantine for a short amount of time instead of the full two weeks, Drejøe said.
The platform has a second functionality that manages and tracks vaccinations in its system. By tracking the product and batch number of the flu shot an individual was administered, any mix-up will be avoided upon the second jab, which they will be notified about through the system. Cure GPS also allows health agencies to update the platform with any new information that emerges about COVID-19 and vaccines and provides a portal for people and medical staff to report any side effects to.
Drejøe added that first line support and development will be done from Nexus, which is located in Houston, Texas and Copenhagen, Denmark
“Within a year or something, you will have a billion … vaccinations done around the globe, so there will be a lot of data to look at, and I think this could provide some valuable insights (because) everything is documented and in the system,” Drejøe said. “Otherwise, … all this super valuable information will be lost… Everybody in the world was taken a little bit by surprise by this one, even though everybody knew at some time it would come. The next one will also come. We know that already, so maybe we can use this as a preparation.”
For those interested in learning more about companies working to provide solutions for COVID-19, TEXGHS will be hosting a Health Security Pitch Event during South by Southwest’s (SXSW) virtual conference on March 18. The event will feature companies, similar to the ones above, that are pitching their COVID-19 response technologies to a panel of judges and will be a great opportunity for people working at the intersection of technology and health security, as well as people in academia, public and private sectors to learn about the startups and innovations of the future.
– Cara Daeschner